Eliminate waste and unlock value in healthcare software spend
By Glenn Landmesser
I’m the digital transformation practice lead for RiseNow. We advise clients on how to effectively digitize supply chain processes.
Many healthcare organizations struggle with declining reimbursement and the rising costs of care delivery. When looking for opportunities to improve operating margins, many hospital leaders strive to increase labor efficiency, optimize documentation, and reduce expenses and waste. In fact, many have built extensive Lean/Six Sigma-trained performance improvement teams to help improve performance and customer satisfaction.
However, one of the larger operational expenses in healthcare (with a larger amount of waste) isn’t scrutinized enough—software licensing and maintenance. It’s time to take a closer look at this waste in healthcare, as indicated by Gartner, Inc. Teams repeatedly see millions of dollars invested in underutilized, sub-optimized software. In this brief overview, I’ll present five reasons for this underutilization and five ideas for eliminating waste and unlocking the hidden value in your software investments.
Five reasons there’s so much waste and “non-value added” in software
Research by Productiv found that large organizations with over 10,000 employees have an average of 364 software applications requiring thousands of interfaces. Being able to eliminate 10% of these licenses could equate to significant savings per year in terms of licensing and interface maintenance costs. While there are many reasons for wasted software investment, the following are five common reasons for underutilization in healthcare:
• Federations. Similar to other industries experiencing mergers, many health systems are a combination of smaller systems that have merged over recent years. This leads to a federated operating model—a collection of associated yet decentralized organizations lacking standardization.
• Regulations. Healthcare organizations are subject to a multitude of rules, requirements and regulations in order to remain eligible for Medicare and private insurance program reimbursement. These ever-changing government and commercial payers’ requirements cannot be met without investment in more software.
• Systematized governance. Only the highest-performing health provider organizations have committed to cross-organizational governance that can objectively evaluate the value of introducing new software into an organization. The chief operating officer (COO) for most organizations is charged with this responsibility. However, it is only natural that they focus just on the most pressing and seemingly expensive decisions.
• Bandages. The redundancies in software capabilities result in doubling or tripling the cost of operations. Rather than leveraging software that’s already in place, vendors often approach leaders and offer solutions to quickly “stop the bleeding” like a bandage.
• User adoption. Lacking quality user adoption programs, many organizations are paying for software and only using limited functionality. As a result, not only is the organization paying for unused software functionality, but it is also wasting money due to workarounds that are deployed to overcome software “deficiencies.”
Five ways to unlock the value in healthcare software spend
There is a lot of money to be saved in an average-sized health system by reducing waste in existing software investments. As is typical with system problems, there is no perfect solution to address underutilized software investments, but here are five solutions that can be leveraged.
• Understand why the pain is occurring. Is technology really causing the pain that needs to be addressed? When evaluating changes in technology, get to the real cause of the “pain.” It might be a poor upstream process.
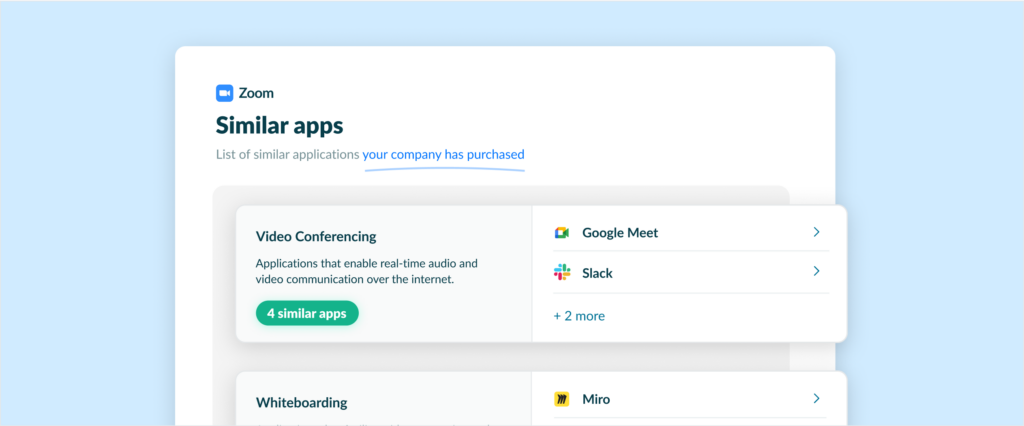
• Cross-organizational check before software purchase. Cross-organizational governance is an important step in unlocking the value of existing technology investments and evaluating future ones. Most health provider systems have established IT governance and service management (ITSM) processes. To improve ITSM, deploy a cross-organizational governance body that understands both business and IT and is familiar with the technology that is already in place.
• Conduct a digital audit. This is the way to know what software is already in place. The governance team should sponsor the annual “digital audit” that creates an inventory of all software applications and licenses (including the business owners, primary users and utilization rates, the total cost of ownership, contract details and the primary use cases) in the organization’s ecosystem. The initial “inventory,” which could be part of a broader application rationalization exercise, is the most painful step but also identifies the most savings.
• Evaluate manual workarounds. Oftentimes, software and spreadsheets are combined to accomplish tasks that could be completed using software alone. Identifying manual processes is a great starting point to look for unused software capabilities. While many users consider spreadsheets a form of automation, exporting and importing data to a spreadsheet indicates there is a problem with the process flow and introduces opportunities for errors. Tools such as Wardley Mapping can help you review the evolution of automation compared to the rest of the industry and develop strategies to close the automation gap.
• Engage your internal performance improvement team. Most hospital systems have built talented performance improvement (PI) teams who are Lean/Six Sigma practitioners. Ask your PI team to help develop visual diagrams to identify functionality gaps and redundancies as well as process interactions. This can support efforts to define the real “pain” and complete digital audits, as described above. The PI experts have been trained to look for the eight kinds of DOWNTIME waste (defects, overproduction, waiting, nonutilized talent, transportation, inventory, motion and extra processing). Add an “S” for the “suboptimal software,” as proposed by Evelina Edmundson as the ninth type of waste, and expand the scope of your PI team to include software optimization in your PI strategy.
Conclusion
If you are looking for ways to return money to your health system’s bottom line, look closely at the waste resulting from underutilized, outdated and redundant software costs. This waste could be occurring due to organizational constructs, financial incentives and governance gaps. Reducing software licensing waste does not require an additional financial investment; it only requires a dedicated and focused approach while leveraging resources already in your organization. In addition, you can find improved user satisfaction, increased productivity and better alignment of technology with strategy and operations.
About Productiv:
Productiv is the IT operating system to manage your entire SaaS ecosystem. It centralizes visibility into your tech stack, so CIOs and IT leaders can confidently set strategy, optimize renewals, and empower employees.
Learn more today